Our experience in saying Goodbye to my Diabetes without using medicine.
Written by Steve and Jennifer Smith. We both wrote this. So the pronouns alternate. Most of it toward the beginning was written by Steve.
We were in the midst of our transition to a new home, so we were between doctors when we started these lifestyle changes. Because we care, we are simply relating to others what we experienced and how reversing diabetes worked for Steve. We made a lot of changes, and we are unsure whether there was one specific habit that changed things most or just a good combination. So, we are sharing all information with you.
We give the same warning to you that we read in several books. If you are on a glucose-controlling medicine now and want to embark on a similar journey, please be sure to monitor your levels often and carefully because these steps in combination with the glucose-lowering meds can bring it down too low. Being under a doctor’s care in decreasing your medication dosages while your levels are decreasing naturally is advised.
=====================================
Through the years, we had gone to health fairs and had blood tests. We had Googled all of the things that came back high or low. We had kind of ignored the ones that weren’t highlighted.
I noticed some black mold in the bathroom stool I used most often. At first, I thought it was something wrong with the water or something growing in the tank part of the toilet. So, we cleaned more often. We also put some of that Tidy Bowl stuff in to hopefully kill off the algae or mold.
Also, my feet started hurting a lot — enough so that it was difficult to sleep. My legs ached.
Finally, in December 2015, I went to the doctor in Nebraska. He smiled and said, “Let’s do some more blood tests, and here is a sample box of Lyrica.” He didn’t say anything about diabetes. Though he wouldn’t have given me the Lyrica if he hadn’t strongly suspected what was wrong. When the blood tests came back, the nurse called and said, “You have diabetes.”
Even though we had suspected it, I had hoped that if I ignored it, it wouldn’t be true.
The black mold in the stool is caused by a high concentration of sugar in the urine. The pain in the feet (“diabetic neuropathy”) is caused by nerve damage. We had kept old health fair blood test results. Now, we went back and looked at them. For several years, my blood sugar was far above what it should have been. The doctor, back then, should have pointed out that I needed to take action. I should have paid more attention to the tests, then. My high blood sugar was not noted as “high” in the alert column on the report, yet it was high according to the range given. So, it was just overlooked by everyone. Note that the “normal range” used on some tests is antiquated. We give a chart later in this write-up that gives the ranges that the medical community is starting to use.
In December 2015, my A1C came back at 13.4. This is very high and is a measure of the blood sugar control over the previous 2-3 months. Anything between 5.7 and 6.4 is considered “pre-diabetic.” Over 6.4 is considered “diabetic.” In truth, “pre-diabetes” is not a grey zone where you don’t need to think too much about it. It is all diabetes, just at varying degrees.
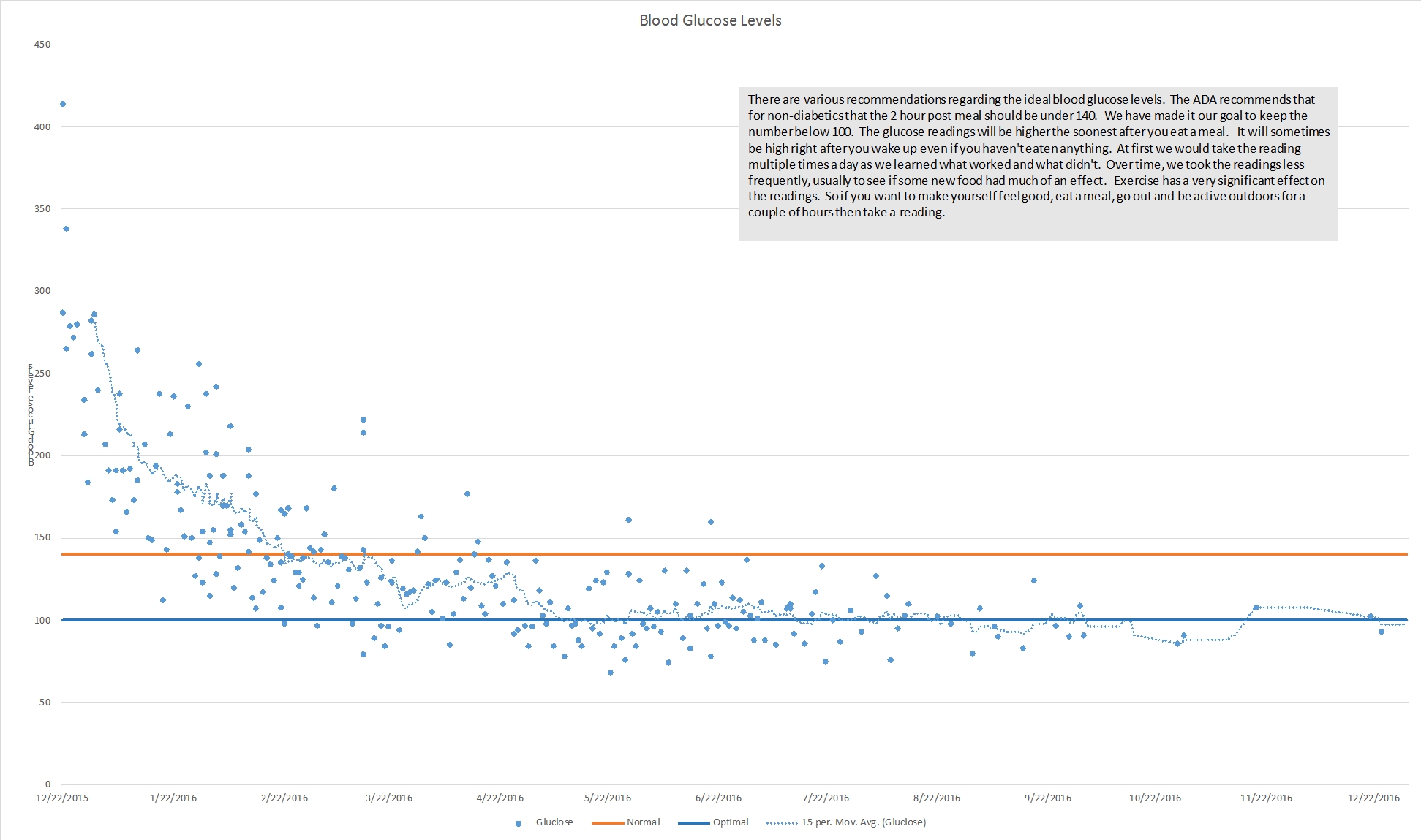
There are a couple of ways you can find out if you are in trouble. There are often health fairs that will test your blood glucose levels as a part of their standard tests. One can request that an A1C test be taken, too. This test shows the 3-month average of your blood sugar control and is probably the best way to tell what is happening in your body. Another way is to find someone with a glucose tester. It will cost them about $0.25 to let you use the tester and one of their strips. Ideally you will want to test your blood about 2 hours after a meal. If you test before that, your sugar will be higher. If you test more than 2 hours after the meal, you could have a low enough number that you think there’s no problem. If the number is over 160, you are diabetic. If it is between 140 and 160, you are pre-diabetic and it is time to start immediately changing some things before you experience the perhaps-irreversible damage you can do to yourself. Now, my 2-hour post-meal number is usually about 100. Ideal is under 100. Before we made the life-saving changes we talk about below, it was often in the 300 and 400 range.
Why is diabetes bad? All kinds of things go wrong in the body. For me, it meant pain in the feet and legs. It meant a very high risk of heart failure and stroke. My blood pressure was high. My cholesterol and triglycerides were high. (Jennifer: My cholesterol and triglycerides were high, too. So, the changes we were about to make were good for me, too.)
For some reason, the statement by the nurse – “You have diabetes” — sparked me to take action. So, we started doing some research.
The chart is big because I am proud of the results from the willpower it took to accomplish this!
Step one for us was to eliminate sugar from the diet. That is hard to do because sugar is in 90% of food in the Standard American Diet. We eliminated sugar substitutes (Splenda, Xylitol, etc), too, since they were noticeably spiking Steve’s blood sugar. This is a decent article about identifying sugars via the ingredients list on the label: https://goo.gl/bB2e2D
We still diligently read labels, but we try to concentrate on eating foods that don’t have labels (i.e. – fresh fruits and vegetables as well as whole grains). I could go through and tell each of the steps of our evolution of our diet but will skip the things that we probably didn’t need to do and will tell you what we have settled on.
At the time of this writing, it has been a year since the diagnosis. Since then, my A1C has dropped down to 5.4! My blood pressure is now on the low end of the normal range. My cholesterol and triglycerides are in the normal range, as are Jennifer’s. My pulse is now normal. My weight is now within the normal range. All of this was done without taking any of the drugs, such as Metformin, that are used by many people to reduce their blood sugar levels. And, there is a reason we wanted to avoid drugs such as Metformin. Long-term, we believe that insulin and other diabetes drugs can make things worse. There are good short-term gains from it, but our research showed lifestyle changes to be far better for long-term control and even reversal of Type II Diabetes.
Within the first month after changing our lifestyle, my blood pressure dropped to normal. That is probably the most surprising thing — how fast my body responded to the changes. Now that my body is within the normal ranges on the tests, we have begun to add back in a few of the foods I have missed in our diet.
I write this up in order to share what has worked for us. I have very good willpower; but the changes we made required every bit of it. I don’t think I would have succeeded without the support and help of my wife. But, the benefits have been worth the changes. I still have the nerve pain and still take a pain medication to help. The Lyrica sample the doctor gave me worked well; but, at $8 a pill and three pills a day, it adds up quickly. I am now using Gabapentin, which costs $0.15 cents a day. Our current doctor told us that whatever nerve damage doesn’t heal within the first year may never heal. We are still hoping for healing, but the remaining effects for me are a very good reason for you to not let your diabetes go on for as long as I did before we stopped it.
Note that I have been a vegetarian all of my life. Being a vegetarian didn’t stop me from getting diabetes and developing very annoying nerve pain. (Jennifer: And, we were still doing some things wrong with our diet.) I had also lived a fairly sedentary lifestyle.
We changed our diet from being vegetarians who would eat anything but meat to a much more fruit, vegetable, and fiber-oriented diet. We changed from a sedentary lifestyle to a much more active one. Our preferred form of exercise is hiking. We often hike several miles a day. Where we live has hills, so some hikes require more energy than others. We make sure that we are active for at least 20 minutes following every meal. We stopped snacking between meals. More on all this later.
Diabetes is caused by the body’s saying, “I have enough sugar, and I don’t need any more.” The insulin that is the key to opening the cell membranes to sugar stops opening the lock. Sugar, then, begins to build up and mess with all kinds of important bodily functions. However, it isn’t necessarily too much sugar in the diet that causes the entire problem. Too much fat is a big culprit. Studies have shown that you can feed one group of healthy people a diet high in sugar and another group of healthy people a diet high in fat. The ones with a high fat diet developed high blood sugar. Those on the high sugar diet did not.
So, why be so watchful of the sugars and foods with a high glycemic load? Part of the reason for that is because processed foods with sugar often have a fairly high fat content. Other reasons are pointed out on sites like this: https://goo.gl/p8zwTc
For our blood sugar goals, we used a chart from Dr. Youngberg’s “Goodbye Diabetes” book, page, 90:
| STAGE 1 | STAGE 2 | STAGE 3 | STAGE 4 | STAGE 5 | ||
| Time From Food Intake |
Optimal Blood Sugar |
High Blood Sugar |
High Blood Sugar |
Prediabetes | Advanced Prediabetes |
Diabetes |
| Fasting | 70-84 | 85-94 | 95-99 | 100-109 | 110-125 | 126+ |
| 1 Hour | 80-119 | 120-139 | 140-159 | 160-199 | 200+ | |
| 2 Hours | 80-99 | 100-119 | 120-139 | 140-159 | 160-199 | 200+ |
The nurse gave me our first blood glucose monitor. The strips can be expensive, but it is worth it to test often while you are figuring out what foods trigger large blood sugar spikes.
Based on our research, as well as testing to see what things affected my blood sugar, the following is what we did and do. It may or may not be “right” for you. But, following this diet and these rules have worked for us. Please also note that part of our research can be found on our Pinterest board:
“Health: Diabetes”
https://www.pinterest.com/snowave/health-diabetes/
The following are some of the guidelines we give ourselves.
- Exercise immediately after every meal for at least 20 minutes. Take a walk around the block. Work in the garden. Clean the gutters. If it is too cold or hot outside, do something in the house like use that exercise machine or do some sit ups and stretches or some kind of exercise routine that moves your body around. Do some household chores. The idea is to slosh the contents of the stomach around long enough that they liquefy and get passed into the small intestine. [Jennifer: From the reading, I gathered it helps the body to process the meal and utilize the new fuel without spiking the blood sugar so much. (smirk)] Do not take a nap. Do not sit down and watch TV. Be active.
- Spend at least an hour each day exercising. For us, that means we often try to do a four mile hike around a lake or something. That takes us a little over two hours. We have other hiking options, and we vary it by taking different trails. For some reason, going on an hour-long hike outdoors lowers the blood sugar more than doing an hour on the treadmill. Besides, it is more fun to get our exercise outside. Note that schools often open up their gyms so you can use their weights or their tracks. There’s also a health club in nearly every community.
- We work at our computers a lot. Sitting for too long is a bad idea. Get up and do something else for a while. I think desk jobs should evict the person from their seat at least once an hour and not let them sit back down for at least 10 minutes. Find something –even a five-minute walk up and down the stairs — that needs your attention.
- Eliminate dairy. This was very hard for me to do. I like cheese. I like butter. I like milk. I miss them. I still miss them. Pizza without cheese isn’t very good. Most cheese substitutes are not good and are an insult to the concept of cheese. But, we eliminated it, and it helped us both.
- Eliminate red meat and fowl. For me, this wasn’t that big of a deal, as I have been a vegetarian all of my life. Loma Linda University School of Public Health has been doing several huge health studies with the largest following 96,000 people since 2002. Forty-eight percent (48%) of the study participants are not vegetarian. Pesco-vegetarians (eat fish) live the longest. Those who eat red meat and chicken live about 7 years less than vegetarians and are much more likely to get cancer.
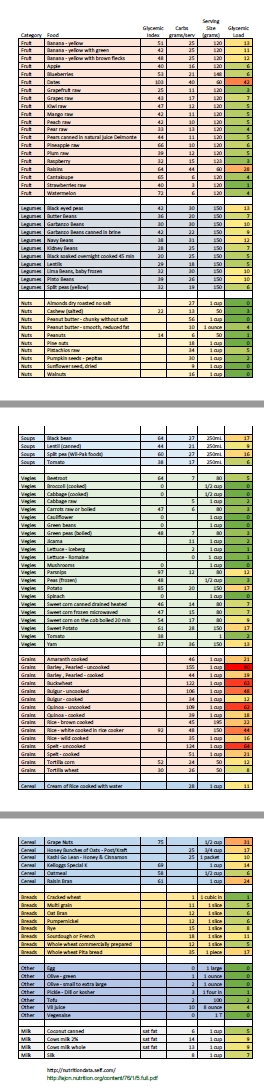
- Pay attention to the glycemic load of foods. Diabetics often refer to a glycemic index which reports how much a cup of a certain kind of food raises the blood sugar of a sample group of people. The glycemic load says that number isn’t that helpful because one should take into consideration the typical portion of various foods. So, instead, it measures the effect on the blood sugar of a typical portion instead of a standard 50 grams. Glycemic loads are not printed on food labels. So, I have compiled my own which has been derived from various sources. It is shared here toward the bottom. While getting my A1C down and stopping the blood sugar spikes, we avoided foods that have a high glycemic load. Now that my A1C is normal, we are introducing a few of the fruits and vegetables with high glycemic load back into my diet, in moderation. [Jennifer: For instance, grapes have a high glycemic load, but we now occasionally eat them, fresh and halved, to sweeten cooked oatmeal. We haven’t reintroduced fresh pineapple yet, but maybe soon.]
- Don’t snack. Learn to embrace your hunger. Consider it a notice that you should do something other than snack. Instead, think of it as a notice to your body to do some chore that needs done that will keep your mind active and thinking of something other than food until your next regular meal. This requires willpower. In time, my body adjusted, and snacking became less of a temptation.
- Eating out is a big challenge. Much of what is on the menu looks very good. Yet, one knows little about what is in the food on the menu. How much fat, how much sugar, etc. does it have? One wants to enjoy the time with friends. Eating out is a great pleasure for many people. Here are some thoughts on it. Carefully consider what you choose on the menu . Realize that eating out probably means it takes longer to control the diabetes. Choose the things likely to have the most fiber and the least amount of fat. Immediately exercise a bit more after eating out than you would if you ate a controlled meal at home.
- If you notice your blood sugar spiking, get to moving and start drinking lots of water. That’s a decent tip in the overall process of getting your A1C levels down, by the way – stay hydrated. We got a couple of water backpacks to take on our hikes. They can be expensive unless you do some frugal and creative shopping. Steve got the backpacks from one company and the water bladder inserts from another.
- What you eat is more important than the exercise. Exercise is important; but controlling what you eat has a far greater impact. It isn’t necessary to strain and stress your body with your exercise routine in order to get good weight control and to reverse Type II Diabetes. Limiting calories and controlling what kinds of foods you eat makes a very big difference.
- One doesn’t need as much protein as the media and “health nuts” sometime tout, but it does help in feeling satisfied between meals. At first, we were vegans, so we eliminated eggs. That probably helped some in bringing my cholesterol levels down. Now, I have maybe four eggs per week. Our other protein sources include beans, nuts, and lentils. There’s a natural peanut butter we found at Costco that’s just ground peanuts. You have to stir the oils into it then keep it in the fridge, but it is better for you than the brand name peanut butters with sugars and, sometimes, added oils.
- We read that a good rule of thumb for how one’s plate should look is one quarter protein, one quarter starchy vegetable or grain, and one half non-starchy vegetables with some fruits.
- Starches: pumpkin, cooked carrot, rutabaga, parsnip, beet root, sweet potato, sweet corn, broad beans, grains (we use kamut as well as “wheat berries”).
- Non-starchy veggies: asparagus, broccoli, brussel sprouts, cabbage, raw carrot, cauliflower, cucumber, endive, garlic, kale, lettuce, mushrooms, onion, peas, peppers, radishes, green beans, spinach, tomatoes, water cress, etc.
- Eat so that it takes a while for your body to process the food. Not only does that help to keep you satisfied between meals, but it also helps to prevent blood sugar spikes. So, how does one do that? Concentrate on getting enough fiber in your diet, preferably via fresh fruits and vegetables. Also, eat whole grains and healthy fats (like nuts and avocado). Steer clear of processed foods, especially as you’re first starting down this path. If a food is already processed or ground to a fine powder (grains turned to flour, for instance), your body will process it quickly and your blood sugar is more likely to spike. Now that my A1C is normal, I am having V8 juice once in a while as well as tomato sauce on things. [Jennifer: We had the V8 and tomato sauce when we first started out, but noticed it was spiking his blood sugar pretty drastically. So, we removed them (and other juices) from the menu for several months.]
- At first, “avoiding the whites” was necessary (white potatoes, white bread, and white rice). Now, mixed in with the high fiber, healthy diet that has brought things back to normal for me, I can eat the occasional potato, have whole grain bread (“Good Seed” bread, yellow label), and black rice every so often.
- We read early in the process that eating something “vinegar-y” with every meal not only balances the acids in your stomach, but also helps your body process the meal without spiking the blood sugar so high. We know it works to regulate the digestive system acids, for Jennifer no longer has to take antacids. We’ve eaten dill pickles or green olives at every meal for a year now. Jennifer often cooks with vinegar, too. It is hard to tell how much of a role it played in bringing my A1C down, but we are trying to mention everything.
- We got part of our ideas from “Goodbye Diabetes” by Dr. Wes Youngberg and a couple of other books. Plus, we read lots of articles and forums online. We watched several videos. We gleaned and pondered as much information as we could about reversing Type II Diabetes and about nutrition.
We put part of what we learned on a couple of Pinterest boards:
https://www.pinterest.com/snowave/health-diabetes/
https://www.pinterest.com/snowave/health-nutrition/ - We’d also read several articles and watched a few videos about the benefit of occasional fasts in order to help your body stop the whole insulin resistance cycle. So, whenever we’d go to the mainland for supplies or some event, Steve would fast for a day or two. I’ve heard recently from a doctor that fasting can put stress on the body, so visiting with your family doc about it first might be prudent. I’ve also read that losing weight “too quickly” can cause gallstones. “People who lose more than 3 pounds per week may have a greater chance of getting gallstones than those who lose weight more slowly.” https://goo.gl/j9U5IU
- If you choose to be vegan for a while, keep in mind you’ll need to make sure you still get all your needed nutrients. Fortified nutritional yeast, flax seed, chia seeds, and Omega-3 fish oil supplements become pretty important. Since I had to stay away from fruit juice (spiked blood sugar) and cranberry is good to protect the kidneys, I take a cranberry supplement.
- Breakfast is our largest meal. Dinner, medium. Supper is our lightest meal.
- Another thing we read early in this journey is how active alpha-lipoic acid (R-ALA) ”has a positive effect on insulin sensitivity, glucose metabolism and diabetic neuropathy.” In Germany, it is used as treatment for diabetic neuropathy. The U.S. is still doing studies on its use for that, but preliminary thoughts are that is might be effective. The effectiveness depends on whether you get pure (R-ALA), synthetic, or a combination. The pure/R is most effective but must be purchased through a “practitioner,” from my understanding. So, we get the combined kind, and Steve takes enough of it that he gets the pure form in the appropriate quantity to do some good. He takes 600mg of the “Doctor’s Best” kind found here (either 3 doses of 200mg or 2 doses of 300mg each day): https://goo.gl/yaAB7t
- Be aware that alpha-lipoic acid can mess with thyroid hormone levels as well as interfere with thyroid medication, if you take it. Also, it might lower the effectiveness of radiation therapy or chemotherapy, even though ALA itself has been shown to fight cancer cells. It is to be taken on an empty stomach, so an hour before a meal or 2 hours after a meal is ideal.
- We placed several articles about ALA on our Pinterest board:
https://www.pinterest.com/snowave/health-diabetes/
- We also learned that magnesium can not only help with sleeping issues but also improve insulin resistance and lower blood glucose levels. So, Steve’s been taking that the last 4 or 5 months of 2016. [Jennifer: Note that, if you take Gabapentin like Steve does, magnesium may decrease the amount of Gabapentin in your blood. So, it is best not to take magnesium within 2 hours of when you take your Gabapentin.]
- There are many foods and spices that may assist your body to lower blood sugar. Some of them are also beneficial for the circulatory system. We use them often in cooking. Here’s a short and certainly not complete list:
- Old-fashioned oatmeal, onions, garlic, mango, chia seeds, turmeric (when used in tandem with black pepper), cumin, mustard, coriander, and cinnamon.
- Controlling inflammation helps in fighting diabetes as well as any neuropathy experienced from having it. Anti-inflammatory foods include:
- Fiber (get at least 25g per day), barley, oatmeal, onions, garlic, leek, scallion, blueberries, bananas (though they are high on the glycemic load; we didn’t re-introduce them until we got his A1C back to normal; even now, though, he gets the greener ones with the lower glycemic load compared to the riper ones), sage, thyme, turmeric, ginger, cloves, cinnamon, rosemary, broccoli, cabbage, brussel sprouts, cauliflower, mustard greens, spinach, flaxseed, kidney/navy/soy beans, extra-virgin olive oil, pistachios, almonds, walnuts, beets, chia seeds.
- Eliminating transfats as well as limiting salt both help in controlling inflammation.
We have now stopped doing the daily records, but we kept them for the first many months to help us learn what worked and what didn’t. The following routine resulted in the gradual loss of about 35 pounds, a normalization of all the important numbers regarding diabetic, weight, heart, and stroke risks.
A sample of our daily records while early in the A1C reducing process:

No, really….here:
2/22
7:00 AM med. alpha-lipoic acid (300mg)
11:00 AM med. cranberry pill
11:00 AM breakfast: tofu scramble (no eggs) with corn on flour tortilla with cashew “cheese” and homemade vegan mayo; 3 green olives; 2 leaves Romaine lettuce; small bowl marion berries; glass of 100% pure V8 juice.
11:00 AM med. 4000 IU D3, chlorophyll, lutein
11:30 AM exercise 2 miles on elliptical
1:15 PM blood test 165
2:20 PM 1 hour, 40 min walk around mt lake. 10,000 steps, 4 miles
4:40 PM blood test first time under 100!! 98
5:30 PM dinner: steamed broccoli with cashew “cheese” sauce; a few almonds, cashews, peanuts; 4 slices dill pickle; 2 PBoas (natural peanut butter, cinnamon, and old-fashioned oats rolled into balls); canned lentil soup (1 bowl).
7:30 PM med. alpha-lipoic acid (300mg)
9:05 PM supper: 1 apple; 1/2 C peanuts.
2/23
3:00 AM med. Advil
3:00 AM symptom foot fatigue and pain; coconut and essential oil massage.
5:30 AM med. alpha-lipoic acid (200mg)
10:30 AM breakfast: red leaf salad greens with 3 green olives, raw pumpkin seeds, and homemade tofu dressing; Apple & cinnamon PBoa bake; jicama.
10:30 AM med. cranberry pill.
11:10 AM exercise 25 min driveway repair and walk down & up the hill.
12:45 PM med. alpha-lipoic acid (200mg)
1:15 PM blood test 140
5:00 PM dinner: homemade chili (1 bowl); jicama; cucumber; thawed green peas; blueberries.
5:00 PM med. 4000 IU D3, chlorophyll, lutein
5:30 PM exercise 30 min driveway & walk down and up the hill. (1 mile now; 1 mile at 11:10am)
7:45 PM blood test 129
8:00 PM supper: 1 homemade TVP taco; jicama; 2-3 PBoas; pistachios.
8:30 PM exercise 2 miles on elliptical, 2.25 on bike at level 9
10:45 PM blood test 168 (TVP gives problems, maybe.)
10:45 PM med. alpha-lipoic acid (200mg)
2/24
7:00 AM alpha-lipoic acid (200mg)
11:30 AM breakfast: Romaine Salad with tomato, artichoke, sunflower & pumpkin seeds, fortified nutritional yeast, 3 green olives; jicama; 1 PBoa; pistachios; 3/4 apple; 100% pure V8 juice.
11:30 AM med. cranberry pill.
12:20 PM exercise 1500 steps on Turtleback Mtn, then walked between library and post office and back. 3500 steps altogether (about 1.5 miles).
2:20 PM blood test 139
2:35 PM med. alpha-lipoic acid (200mg)
4:35 PM dinner: cashew taco (not to be repeated)[Jennifer: There were a few experiments. I’m working on recipes. (grin)]; red leaf lettuce with some homemade tofu dressing; tomato; small bowl (3.1 oz) marion berries; 2 PBoas; 3 slices dill pickle; some peanuts; 1/2 C leftover tofu “quiche” with corn (no eggs).
4:35 PM med. 4000 IU D3, chlorophyll, lutein
7:40 PM blood test 142
7:50 PM med. alpha-lipoic acid (200mg)
8:20 PM med. Advil
8:20 PM symptom legs weary and fatigued ever since Turtleback Mtn walking; sensation of burning on feet.
10:45 PM symptom hurting shin (left); massaged calves first, then coconut/essential oil massage to shin.
2:00 AM sleep Slept from 11pm till 2am.
2/25
10:00 AM med alpha-lipoic acid (200mg)
3:00 PM blood test 129
3:15 PM dinner: 1 can lentil soup; jicama; 1 dill pickle; 1.5 apple; 2 handfuls peanuts; 3 almonds.
3:15 PM med. 4000 IU D3, chlorophyll, lutein
4:00 PM exercise 1/2 mile stationary bike; 1.5 miles elliptical.
5:55 PM med. alpha-lipoic acid (200mg)
7:15 PM supper: Romaine salad with tomato, artichoke, green olives, spices, sunflower and pumpkin seeds, onion, fortified nutritional. yeast, and salt/vinegar roasted chickpeas; pistachios.
8:00 PM exercise dishes; stretching; walking around; sit-ups; snowballing defenseless wife.
10:30 PM med. alpha-lipoic acid (200mg)
2/26
4:40 AM med. alpha-lipoic acid (200mg)
11:11 AM med. alpha-lipoic acid (200mg)
11:30 AM exercise walked around town a bit; 2900 steps; 1.3 miles.
1:30 PM dinner: cucumber/tomato/onion/vinegar/vegan mayo salad; broccoli/cauliflower/sunflower seed/vegan mayo/basil/vinegar salad; 1 PBoa; 1 piece jicama; 4 strawberries; small glass 100% pure V8 juice.
1:30 PM med. 4000 IU D3, chlorophyll, lutein
2:20 PM exercise dishes; 35 min, 5 miles on bike and elliptical
4:24 PM blood test 121
7:11 PM food: 1 bowl clear mushroom/onion soup with fortified nutritional yeast; cherry tomatoes; jicama; pistachios; 1 bowl blackberries; 1 dill pickle.
8:00 PM exercise bike 1.75 miles; 1.5 on elliptical.
9:00 PM symptom NO FOOT PAIN TODAY AND YESTERDAY!; only slightly irritated on top tonight, but nothing compared to the way it has been for months. YAY!
9:30 PM med. alpha-lipoic acid (200mg)
10:00 PM blood test 129
2/27
6:00 AM blood test 125
6:00 AM breakfast: 1 bowl homemade chili; 1 slice sourdough bread; 1/2 avocado; orange.
6:00 AM med. cranberry pill
6:30 AM exercise 30 minutes on bike, 5.5 miles
9:30 AM med. alpha-lipoic acid (200mg)
9:30 AM blood test 138
12:00 PM dinner: 2 PBoa; jicama; romaine salad with tomato, onion, green olives, sunflower and pumpkin and flax seeds, and too much Real Salt; edamame (probably 1/4 cup).
12:00 PM med. 4000 IU D3, chlorophyll, lutein
12:30 PM exercise dishes; walk around book sale and Village Plaza.
3:45 PM supper: 1 bowl homemade chili; jicama; strawberries; pistachios; some cashews.
4:20 PM exercise total steps for day = 7900; walked to Day Lake and back.
6:10 PM med. alpha-lipoic acid (200mg)
9:20 PM med. alpha-lipoic acid (200mg)
2/28
6:00 AM med. alpha-lipoic acid (200mg)
7:30 AM breakfast: 1 bowl homemade chili, 1 dill pickle, half can sweet corn, 1 bowl blueberries, almonds.
8:15 AM exercise 1 mile bike, 2 miles elliptical
1:30 PM dinner: Jicama; cantaloupe; 2 PBoa; 3 grapes; small bowl roasted brussel sprouts; 6 green olives.
1:55: PM exercise 3.7 miles on elliptical, 25 min.
5:00 PM med. 4000 IU D3, chlorophyll, lutein
5:00 PM supper: finished eating at 5:45 ; 2 falafels (flour tortilla with chickpea & spices, tomato, romaine, vegan mayo); cashews; almonds; apple (1.5).
5:45 PM exercise dishes; stretches; sit-ups; throwing snowballs at wife in despicable manner.
7:20 PM med. alpha-lipoic acid (200mg)
7:20 PM blood test 168
10:25 PM med. alpha-lipoic acid (200mg)
2/29
2:30 AM med Advil
9:15 AM breakfast: blueberries; flour tortilla spread with avocado/cashew “cheese”/vegan mayo then stuffed with salad of Romaine, green olive, onion, green peas, edamame, tomato, and flaxseed; jicama; 1 seed PBoa.
11:30 AM exercise 15 min elliptical; weight lifting (2 rounds on gym equipment).
12:30 PM med. alpha-lipoic acid (200mg)
12:45 PM blood test 144
1:30 PM food: homemade falafel waffle mixed with tahini/lemon/garlic sauce with salad combo from breakfast; 1/2 dill pickle; jicama; 3 seed PBoa; some pistachios; 1 apple; 4 strawberries.
2:05 PM exercise walk down driveway and back.
2:40 PM med Advil (back pain in area where kidney stone had been)
5:45 PM med. alpha-lipoic acid (200mg)
7:30 PM food: Italian-roasted Cauliflower, 2 seed PBoas; 1/2 apple; 4 green olives; 1 bowl blueberries.
7:30 PM med. 4000 IU D3, chlorophyll, lutein
8:00 PM exercise laundry; stretching; sit-ups; walking around.
10:00 PM med. alpha-lipoic acid (200mg)
• Not long after this, we eliminated the TVP, bread, and V8 juice for a while as well as exchanged the flour tortillas for whole grain tortillas. We also added kamut, wheat berries, chia seeds, and much more old-fashioned oats to get more grains. Finally, we added even more use of beans for not only the fiber but also to help with satiety between meals. As a result, we saw lots of improvement in his glucose levels. Wonderfully, his A1C started dropping and continued to do so until it is solidly in the normal range!
This is a pdf version of the glycemic load reference sheet that I created. It is easy to print and use. We posted it on our fridge to help us decide what to eat or not. Click on this for the printable pdf file … Glycemic
Why you don’t want diabetes
This is a good article about “prediabetes” and insulin resistance, what causes them, and what reverses them:
https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance
You don’t want to get to any stage of diabetes. And, if you have gotten there, you want to reverse it. Diabetes affects all of your body — every organ and cell.
At least 65% of diabetics will die prematurely from complications associated with cardiovascular disease, caused by damage to the circulatory system. (Dr. Wes Youngberg)
Rather than wait to start having the negative symptoms, it is far better to take action to make sure you don’t have the problems in the first place. I wish I had not waited until I had nerve damage before I acted. I was at a high risk of having a heart attack or stroke because of my spiking blood sugar, high blood pressure, high cholesterol and high triglycerides. My body was struggling with inflammation and resisting insulin. Our bodies were deteriorating.
What diabetes (all kinds) can cause:
Nerve Damage – this means pain and more injuries. In my case, the nerve damage caused my feet and legs to hurt enough that I couldn’t sleep. The reversal of the diabetes, Gabapentin, and oil rub are helping. Time will tell whether the damage already done will heal.
Vision Loss – much higher chance of vision-related problems. In my case, I frequently got iritis (a form of uveitis). It can be treated with steroids; but the more steroids you take, the more likely you are to get glaucoma and other damage.
Kidney Disease – About 180,000 people a year have kidney failure because of diabetes. Fortunately, my kidneys are fine; but, you definitely don’t want your kidneys to fail. They are rather important.
Amputation from Peripheral Vascular Disease – One of the more common problems with diabetes is the failure of the small capillaries that transport blood. Hands, feet, and legs often suffer. My grandmother had her leg amputated for this reason.
Heart Attack – Those with diabetes often have high cholesterol and weight problems that significantly increase the chances of heart attacks.
Stroke – Because of the damage to the small blood vessels, the chances of an aneurysm are significantly increased.